Antipsychotics are alike, but their similarities are different
It had been a long day for some delegates at the ECNP by the start of this symposium on Sunday evening. Nevertheless, the large audience was educated by a panel of four expert speakers who discussed the current state of the art in managing psychosis.
Is there something toxic about having schizophrenia?
Professor Robin Emsley of the University of Stellenbosch, Cape Town, South Africa set the scene, by describing the evolution of pharmacological treatment for schizophrenia. The effect of current treatments means that, when patients engage well with their therapy, outcomes are usually extremely good for patients experiencing a first episode of schizophrenia. These symptomatic benefits are most pronounced in the first 6 months of treatment. After this time, the focus needs to shift from symptom remission to the prevention of relapses as well as on optimising patient’s functioning, as these place such a burden on patients and their caregivers and prevent patients from fulfilling their individual goals. Moreover, for many years, results have indicated and researchers have speculated about the possibility that relapses have neurotoxic effects on the brain, and relapses may be a critical factor in the development of treatment refractoriness and poor long-term outcomes in schizophrenia.
Just can’t take this feeling anymore
One important factor in avoiding treatment relapse is medication adherence, Dr Leslie Citrome of the New York Medical College, USA, pointed out. This often comes down to tolerability. When making treatment decisions, Dr Citrome advised, the clinician needs to take into account the known common side-effects of available antipsychotics, but also the patient’s past medical history and response to medications, all of which might limit the choice. One way to reduce unwanted effects of medications such as extrapyramidal symptoms (EPS) and sedation is to choose agents bearing in mind their side effect profile. The psychiatrist needs to listen to the patient’s experience of the medication, and their needs and desires in terms of tolerability. Shared decision-making is key to promoting adherence.
The same, but different
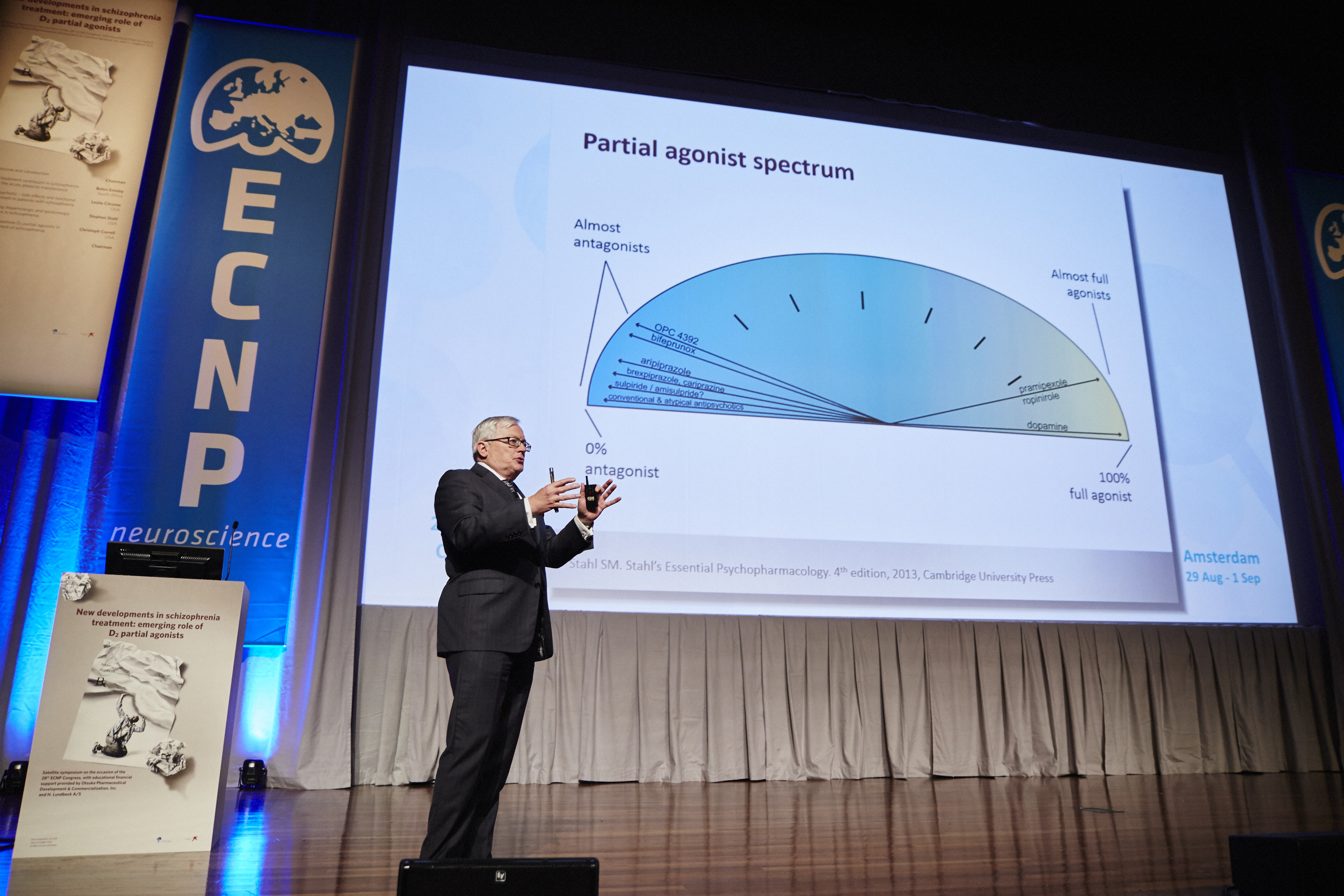
Antipsychotics are alike, but their similarities are different, was the paradoxical way in which Dr Stephen Stahl, of the University of California-San Diego, USA, introduced his presentation. Primarily, antipsychotic effect is related to occupancy of the dopamine D2 receptor, but it’s not all about a medication’s binding to this site. The atypical antipsychotics bind to dozens of different neurotransmitter receptors, and none of their receptor profiles are identical to each other. The feature that these compounds share is that they all bind to D2, and to at least one of the serotonergic receptors, but that is where these broad similarities end.
Dr Stahl presented, in a creative way, an illustration of receptor-binding profiles of various antipsychotic agents. In addition, within the family of antipsychotics, many of the second-generation have potent effects as 5HT2A antagonists and/or as 5HT1A partial agonists / agonist, both of which have effects in reducing EPS. In addition, some of these antipsychotics have in common partial agonism of the D2 receptor, rather than the full antagonism that is a feature of antipsychotics, but also show distinct receptor binding profiles which may translate into different clinical characteristics
Hitting the sweet spot
Dr Christoph Correll, from the Zucker Hillside Hospital, New York, USA, continued this theme of receptor-activity profiles of the antipsychotics. The change in intrinsic activity at the D2 receptor from antagonism to partial agonism was one that has long been sought and researched, as it gives the option for not simply switching the receptor on or off, but maintaining a balance of activity that may help restore more physiological levels of functioning in different parts of the brain. Dr Correll talked about a ‘sweet-spot’ between agonism and antagonism. However, the challenge is that this is not fixed, either in different parts of the brain, or when the brain is in different states with varying levels of dopaminergic activity. The trick for therapies that are D2 partial agonists is to strike the balance in enough areas of the brain, under enough physiological conditions, to produce the desired therapeutic effects.
As Prof Emsley concluded, blockade of the dopamine D2 receptor remains a necessary and sufficient condition for antipsychotic efficacy. However development is moving towards finding more sophisticated ways of modulating the multiple receptors that are involved in the development and management of schizophrenia.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Otsuka and Lundbeck.


