





L'età di esordio del disturbo bipolare può giocare un ruolo importante nel decorso a lungo termine della malattia. I maggiori esponenti della psichiatria, sottolineano l'ultima ricerca in questo cempo, nonchè l'importanza di questo tema nella pratica clinica.
Prof Giovanni de Girolamo, from IRCCS Fatebenefratelli, Italy, presented key reasons for why the age of onset of bipolar disorder is relevant and important. Firstly, it allows us to study the precursors and prodromes of the disorder; as well as the lifetime risk and comorbidities. But most importantly, it enables us to plan primary and secondary prevention, and early interventions.
One of the first questions to ask, Prof de Girolamo told us, is: what does ‘age of onset’ mean? This may not be as simple as it sounds. It could mean one of several things, including the age when the first signs of a disorder appear (e.g. cognitive dysfunctions), or the age of the first pharmacological treatment. There are in fact several, heterogeneous criteria to define the age of onset.
Currently, there are no widely agreed definitions of the onset and initial management of bipolar disorder, and the effect of treatment delay on the outcome of bipolar disorder is unknown. Prof de Girolamo and colleagues undertook a meta-analysis to look into the interval between the onset and the initial management of bipolar disorder. Twenty-seven studies were identified from 5,785 articles using pre-defined selection criteria, and were included in the quantitative analysis. The studies were conducted all over the world, including the USA, Spain, Turkey, Australia, Thailand, France and Italy.
While there was very high between-sample heterogeneity, it was found that the pooled interval between the onset of bipolar disorder and initial management was almost six years! Using sensitivity analysis of the onset definitions, it was shown that the interval for first symptoms, first episode and illness onset were 5.4, 6.8 and 4.2 years, respectively.
The onset of bipolar disorder and initial management was almost six years!
Prof de Girolamo proposed that the marked variation between the studies was partly explained by the way in which onset was defined, how the chronology of onset was assessed, the average age of onset, the proportion of patients with bipolar disorder I and when the study was published.
Regardless of the heterogeneity observed, the clinical implications are clear: even in research centers, there is an unacceptably long interval between the emergence of symptoms and the identification and treatment of bipolar disorder. This study identifies an opportunity for intervention in the early stages of illness, which may in turn postpone or prevent the progression of bipolar disorder.
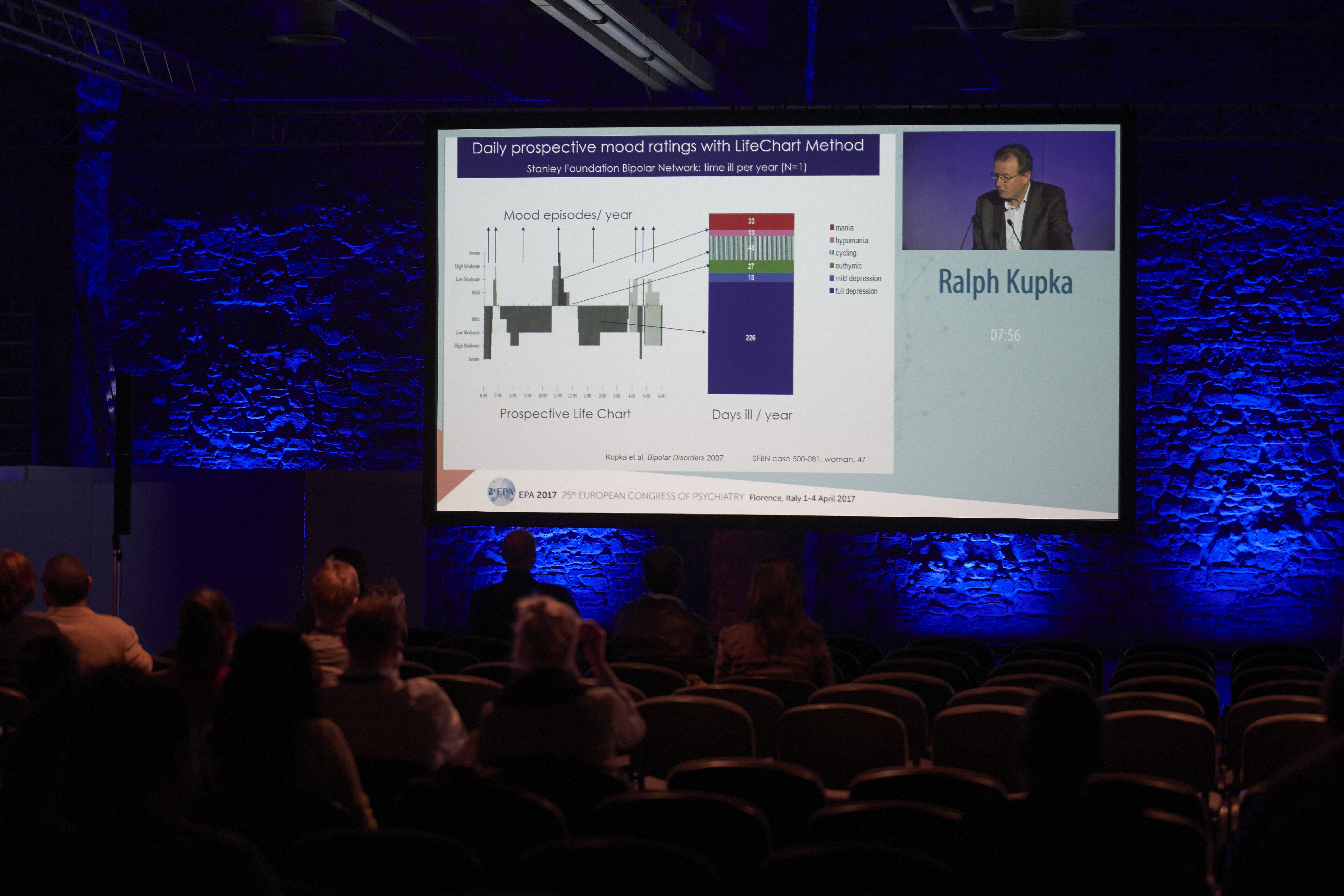
Prof Ralph Kupka, VU University Medical Center, The Netherlands, described the impact of age of onset on subsequent illness course and relevant findings of the Stanley Foundation Bipolar Network (SFBN).
Prof Kupka emphasized the point made by Prof de Girolamo, that there is huge variation in the definition of the age of onset of bipolar disorder. This is partly because a diagnosis of unipolar depression may precede the first manic episode by years - even decades - at which time a diagnosis of bipolar disorder would be considered. Data from 7 studies, including 2,968 patients, highlight that a large proportion of patients with bipolar disorder are diagnosed between 15 and 19 years of age. Of the 539 patients included in a study by the SFBN, the mean age was 42.5 years, with a mean age of onset of 23.4 years. Approximately 32% of patients experienced their first symptoms of depression and mania at the same age, and 15% experienced mania first. In contrast, over 53% of patients had depression first. Prof Kupka pointed out a patient who first suffered from depression as a teenager, but only reported symptoms of mania when he was over 65 years of age! This makes determining a ‘start date’ difficult.
A particularly interesting finding from the SFBN is that before the age of 20 years, the percentage of positive family history of bipolar disorder was much higher (over 60%) compared to those with an age of onset of over 45 years (approximately 25%). Prof Kupka proposed that genetic loading may play a greater role in early onset bipolar disorder, compared with late onset. In addition, data from the SFBN showed that physical and sexual abuse in childhood play a role in earlier age of onset of bipolar disorder. Verbal abuse in childhood was also associated with an earlier onset and more difficult course of illness.
Prof Kupka concluded that SFBN-data reveal that an earlier age of onset is associated with a poorer long-term outcome - more depression, mood instability and rapid cycling- as well as a longer delay to first treatment. However, he pointed out that other studies have not found a significant association between age of onset and severity of mania, psychotic features or rapid cycling.
It seems that the evidence of a negative impact of an early age of onset on the longitudinal course of bipolar disorder is inconsistent.
The evidence of a negative impact of an early age of onset on the longitudinal course of bipolar disorder is inconsistent.
Prof Philippe Conus, Lausanne University, Switzerland, concluded the session with a perspective on the impact of age of onset on the first episode of psychotic mania. At the Early Psychosis Prevention & Intervention Centre (EPPIC), 87 patients with first episode psychotic mania were followed for 12 months. The age of entry to the EPPIC was looked at as one of the predictors of outcome. Using the onset age cut-off of 21 years, it was found that age was not correlated with outcome characteristics.
The impact of sexual abuse featured again in the symposium as it was noted that sexual trauma played a greater role in later age of onset of any mood disorder. Prof Conus proposed that early onset bipolar disorder is more biologically driven, i.e. genetics play a bigger role; whereas later onset disease is more often triggered by life events, such as abuse.
Prof Kupka pointed out that this finding may be contradictory to his conclusions, in which sexual abuse and a family history of disease was associated with earlier onset. A possible explanation is that Prof Conus only looked at psychotic symptoms, i.e. patients who were admitted to the EPPIC, not all mania patients, and so these data may represent a specific subgroup of patients.
The insightful discussions throughout this symposium highlight the need for ongoing research in this field. Crucially, patients’ needs may be different depending on the age of their first treatment.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.