Effective treatment of depression enables a return to a pre-depression lifestyle
Treating major depressive disorder (MDD) effectively to enable patients to return to their pre-depression performance at work and at home is one of the highest priorities in mental healthcare. Experts from Spain, Australia and Canada explained how best to achieve, and how to evaluate this at EPA 2018.
Treatments for depression work. This was recently confirmed by the ground breaking, comprehensive network meta-analysis of short-term studies published in the Lancet in February 2018.1
Further evidence for the effectiveness and tolerability of antidepressants when used by patients in everyday clinical practice is also being provided by long-term and real-world studies, said Eduard Vieta, Professor of Psychiatry at the University of Barcelona, Barcelona, Spain.
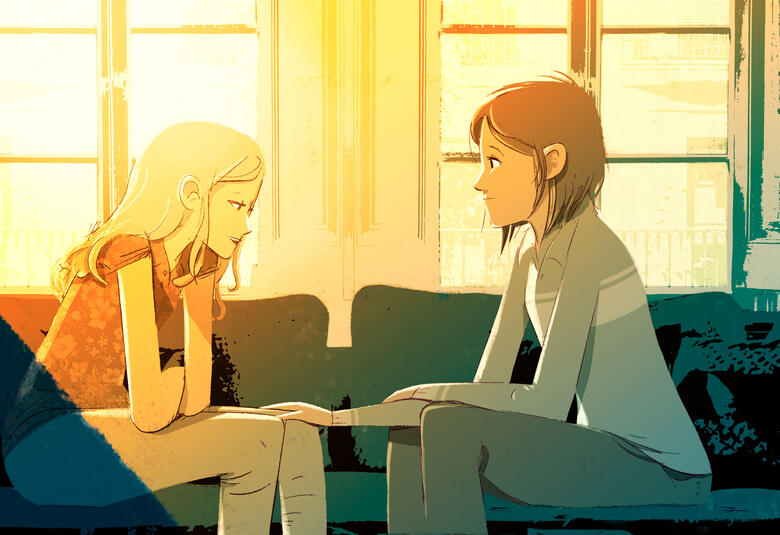
Major depressive disorder (MDD) results in the highest disability burden of all mental health disorders.2 Treating it effectively to enable patients to return to their pre-depression performance at work, at home and in their social life is one of the highest priorities in mental healthcare, Professor Vieta said.
Treating MDD effectively to enable patients to return to their pre-depression performance at work, at home and in their social life is one of the highest priorities in mental healthcare
The definition of treatment success in depression has evolved
Professor Vieta described how, in the 1970s, a response to treatment was the goal. This was defined as a reduction of symptoms (e.g. ≥50% Montgomery-Åsberg Depression Rating Scale (MADRS) or the Hamilton Depression Rating Scale (HAM-D) score, so many symptoms remained.3,4
By the 1990s, remission was the aim, and was commonly defined as MADRS score ≤102 or HAM-D17 score ≤7.4,5 However, nearly half of depressed patients who achieve ‘remission’ according to scale or clinical definitions do not consider themselves to be in remission.2,4
To reconcile the emerging views of patients and clinicians we need to go beyond the traditional views and outcomes
In 2018, the therapeutic aim strives for full functional recovery without symptoms that enables the individual to return to a pre-depression lifestyle. Its achievement is confirmed by direct questioning combined with a clinical impression to assess patient-specific function and quality of life.6 Importantly, this therapeutic aim aligns with that desired by patients.7
How to achieve a full functional recovery
Professor Vieta discussed how to achieve a full functional recovery therapeutically based on the published evidence.
He pointed out, however, that the most commonly used tools to assess the effectiveness of therapy for depression, such as the MADRS and the HAM-D, were designed before the importance of identifying and treating cognitive symptoms in depression was fully appreciated. Of note and of the ten sections in the MADRS, only one (concentration difficulties) focuses on cognitive ability.8
Despite these limitations, meta-analyses provide useful knowledge on the comparative efficacy (response rate) and acceptability treatment discontinuation) for new-generation antidepressants,8 said Professor Vieta.
This has been demonstrated by Andrea Cipriani and his colleagues,1 who have carried out the largest, most robust analysis of the comparative efficacy and acceptability of 21 antidepressants used as an acute treatment for adults with MDD. The study included 522 trials and 116,477 patients. All antidepressants tested were more effective than placebo. The differences between individual antidepressants (particularly in placebo-controlled studies) in terms of efficacy and acceptability were relatively small.
Professor Vieta highlighted, however, the importance of post-hoc analyses of long-term treatment to assess tolerability, compliance and adherence.9
The clinical relevance of cognitive and functional measurements in MDD
Patients with residual symptoms relapse earlier and are three times more likely to relapse than patients without residual symptoms.10
Clinical symptoms within the cognitive domains of executive function, attention, memory and processing speed lead to functional impairment, explained Bernhard Baune, Professor of Psychiatry, Royal Adelaide Hospital, University of Adelaide, Australia.
At diagnosis, 68% of patients with MDD have severe functional impairment.11 Professor Baune emphasized the need to address this impairment,12 in addition to remission of depressive symptoms to achieve a full recovery.
The new paradigm is to do our best to make our patients not just feel well, but do well.Feeling well and doing well leads to being well
However, Professor Baune noted that the evidence regarding the comparative effectiveness of antidepressants on cognitive symptoms is limited. Very few antidepressants demonstrate statistically significant improvement on cognitive testing using the Digit Symbol Substitution Test versus placebo and versus specific antidepressants.13
Studies of the real-world effectiveness of antidepressants complement the more traditional RCTs required by regulatory bodies, said Pratap Chokka, Clinical Professor of Psychiatry and Consultant Psychiatrist, University of Alberta, Alberta, Canada.
Real-world studies provide broader information on the long-term effectiveness and tolerability of antidepressants and the associated compliance and adherence to treatment in circumstances that more closely reflect real-life settings, including clinical practice.
Professor Chokka highlighted the AtWoRC (Assessment in Work productivity and the Relationship with Cognitive symptoms) study as an example. This is a recently completed interventional, open-label, Canadian study in employed patients with MDD treated with an antidepressant with demonstrated efficacy in cognition.
Improvements in cognitive symptoms of depression lead to improved workplace productivity
The results showed a strong association between improvements in the cognitive symptoms of depression and improved workplace productivity,14 reinforcing the need to address the cognitive symptoms of depression to improve functional outcomes.
This satellite symposium was sponsored by Lundbeck and presented at EPA 2018.