‘Biomarkers in the clinic - are we there yet?’
Following the ECNP’s special meeting on biomarkers in the clinic held in March, details of some of the most promising candidates were presented during this interesting and well-attended session. As the session’s co-chairman Shitij Kapur, UK, pointed out, “Biologists owe clinical psychiatrists big time – we’ve been promised clinical markers for mental illness for 30 years”. But are there still no management guidance tools or diagnostic tests? Excitingly, this session suggests things may be coming to fruition after such a long wait.
Three of the most promising areas under investigation in the search for biomarkers were discussed; machine learning, informational processing and premorbid functioning, and referral markers.
Psychosis – external validation is key
Dr Paolo Fusar-Poli, UK gave a current assessment of the state of play in the field of stratifying patients at risk of psychosis. Currently, there are no validated markers or clinical tests to assist in the diagnosis or treatment of psychosis. However, that doesn’t mean that the field is dormant – far from it. Considerable effort is being expended in the search for biomarkers to aid in the identification of psychosis and, importantly, the identification of those at high-risk of developing psychosis.
Three of the most promising areas under investigation in the search for biomarkers were discussed; machine learning, informational processing and premorbid functioning, and referral markers. While individual departments report some success in identifying possible biomarkers in psychosis, external validation of biomarkers is a key challenge that needs to be addressed together with the standardisation of assessment tools. Hopefully, the PSYSCAN trials, large studies dedicated to stratifying risk of psychosis and which are being undertaken in UK, Germany and US, will go some way to support the accurate replication and validation of psychosis biomarkers.
Major depression – personalised medicine realised
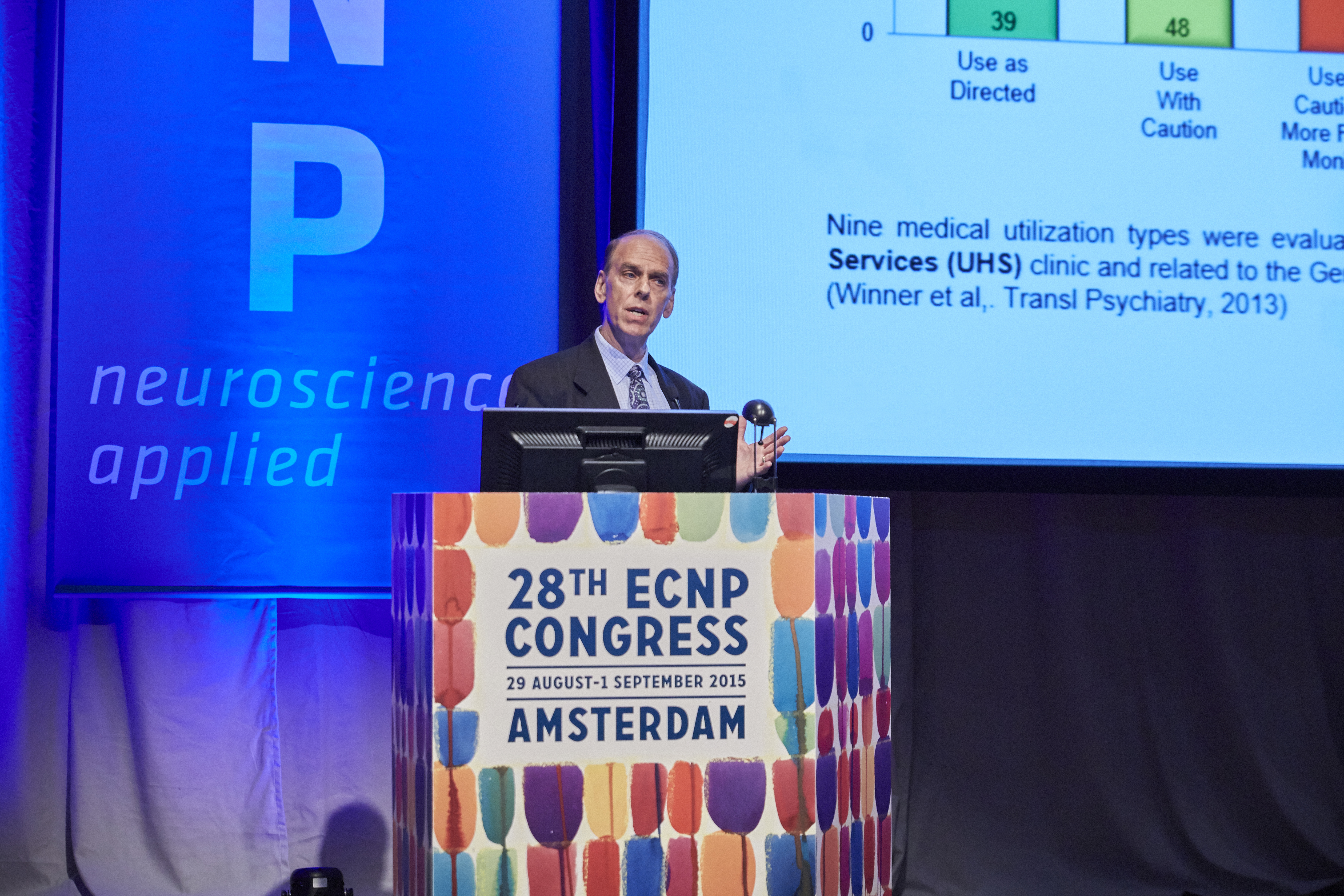
Dr C. Anthony Altar, GeneSight, Ohio, USA explained how the examination of just 8 genes and 47 single nucleotide polymorphisms (SNPs) in a combinatorial approach can assist psychiatrists in the prescription of therapies for major depression.
In this pharmacogenomics investigation, the key is in selecting the correct SNPs. Those chosen were in the genes for enzymes responsible for the metabolism and degradation of therapies frequently used in the management of major depression. For example, it is known that variations (due to SNPs) in the CYP2D2 genes of patients being given a specific antidepressant affect the dose response curve, with some patients metabolising it rapidly, thereby depleting therapeutic levels quickly, while other patients metabolise it more slowly, thereby maintaining therapeutic dose levels for longer. By examining the metabolic profiles of a number of different drugs and correlating these with the combined cytochrome SNP data from patients with depression, Dr Altar explained how it is now possible to generate an interpretative report that predicts the appropriateness of a particular drug for a particular patient, thereby guiding a physician’s choice of treatment. In particular, the report flags when certain drugs should be used with caution.
Benefits not to be SNP’d at
This innovative approach has been verified in 3 prospective double-blind randomized control trials (RCT). Each evaluated use of the gene pharmacogenomic test and interpretive report for the management of psychotropic medications used in the treatment of major depression in an outpatient psychiatric practice compared with use of the usual therapies. Pharmacogenomic-guided treatment significantly increased the likelihood of response in all patients with treatment resistant depression and identified many patients with severe gene-drug interactions who, when switched to genetically ‘suitable’ medication regimen, experienced great improvements in their depressive symptoms. Such an approach has also been shown to afford significant cost-savings in the management of major depression.
The future’s digital for mood disorder management
“We are more diligent about ensuring that our mobile devises are charged than we are about ensuring our children are fed!” said Dr Paul Wicks, in his introductory remarks to a fascinating talk about the immense potential digital technology has in the assessment and management of mood disorders. Already, the search term ‘mood tracker’ yields hundreds of hits and many self-help apps are available that claim to help assess mood, even using biosensors in smart phones to do so. Sadly, of those apps examined more thoroughly, none appeared to be clinically accurate; the app provider it would appear expends more effort ensuring the programme is user-friendly than that the actual advice being given is correct. None the less, the fact is that apps are quick and simple to use and their development time compared to an RCT is rapid, to say the least. And they are popular. Leveraging digital technologies in the future to help those with mood disorders could be highly beneficial. “Consider Facebook,” said Dr Wicks, “1 billion people log in to Facebook daily. We don’t need to do too much that, with the right approach, we could do some good.”
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.