Artificial intelligence offers new perspectives on psychiatric diagnoses
Computational neuropsychiatry is a new discipline, exciting huge interest for its potential in diagnosis and possibly even management. Progress in Mind had a unique opportunity to interview Dr Mitsuo Kawato, of the Advanced Telecommunications Research (ATR) institute International in Kyoto, Japan, ahead of his plenary lecture at CINP2016 on this intriguing subject. We report on his presentation and shared insights.
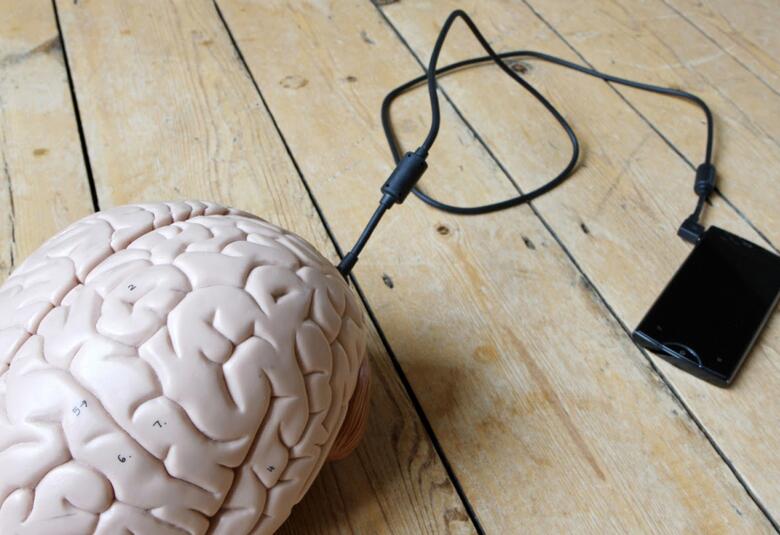
Artificial intelligence is a term that conjures up images of robots and machines capable of intelligent thought. In the field of psychiatry, artificial intelligence principles and practices are being used to take neuroimaging data and develop biomarkers that could support a clinical diagnosis and quantify and describe that diagnosis.
Neuroimaging biomarkers
Dr Mitsuo Kawato of the ATR Computational Neuroscience Laboratories in Kyoto, Japan, has been involved in research that for the first time defines the biological dimension – an imaging dimension – of a psychiatric diagnosis. Research published by Dr Kawato and colleagues in Nature Communications in 2016 ranked among the top 1% of viewed scientific papers published in same period. Dr Kawato believes this is because the paper dealt with an artificial intelligence application that could define autism spectrum disorder (ASD) using neuroimaging-based classifiers – or biomarkers. The research team are using the application to define and create neuroimaging biomarkers for major depressive disorder (MDD), schizophrenia, obsessive compulsive disorder (OCD) and chronic pain syndromes.
Taking data from 200 patient samples, and looking at 10,000 neuroimaged connections and 140 brain lesions, Dr Kawato said it had been possible, using sophisticated artificial intelligence algorithms, to select the 16 functional connections that are specific for and discriminate ASD from normal (typically developed) brains. He explained that this type of computational neuroscience allows the description of one scale – one dimension – that plots the Gaussian distribution for typically developed individuals and another that plots the distribution for, in this case, ASD. This biomarker tool therefore also allows for a quantitative assessment – or score for the diagnosis.
Distinctions and connections
What is more, Dr Kawato explained that these neuroimaging biomarkers being developed not only define and describe a specific diagnosis, but highlight distinctions between diagnoses and similarities and closeness of certain diagnoses. For example he said that the ASD neuroimaging biomarker could not distinguish MDD patients from their controls, but showed some ability to discriminate between patients with schizophrenia and controls. According to Dr Kawato, this closeness between ASD and schizophrenia is in keeping with historical views that these conditions shared some commonality and with genetic studies indicating common loci for schizophrenia and ASD.
Dr Kawato believes that neuroimaging biomarkers will be a valuable support to clinical diagnosis and will become a reality of practice and diagnosis in the near future. He told Progress in Mind: “In other disciplines of medicine like cardiovascular medicine and oncology for example, it is common to examine biomarkers – be they blood biomarkers or imaging scans (fMRI and PET). But in psychiatry, we haven’t had that kind of quantitative measurement to support the clinical diagnosis.”
“We had two objectives. The first was to provide objective scales to support clinical diagnosis with neuroimaginging based biomarkers.” Dr Kawato then said that if these biomarkers prove to be really reliable, it may be possible to use these tools to explore and describe the neurocircuits and brain regions with correlates for predicting certain diagnosis.
Resting state data
Dr Kawato described how the neuroimaging biomarker looks at resting state fMRI, with a 5-10 minute scan providing the data to allow a quantitative diagnosis. He said that in the future it might be possible, not just to diagnose one condition, but to use all the available biomarker scales to see if, in the case of ASD for example, a person has a condition more predominantly located between ASD and schizophrenia – or located closer to the normal healthy position.
Biofeedback
These developments in neuroimaging biomarker research might also have applications in the management of psychiatric disorders. Dr Kawato said that real-time feedback based on imaging biomarkers might have therapeutic applications in some diagnoses. He explained: “We can define “ASDness” and then in realtime we can feed this back to our patient as a score. It’s something a bit like cognitive behavioural therapy or psychotherapy, although a little bit more high tech.” Dr Kawato said that pilot studies in ASD, MDD and chronic pain conditions, have been looking at this real-time feedback. According to Dr Kawato, outcomes may depend on the learning capability of a given patient and some conditions may be more amenable to reinforcement conditioning than others.
For the future, Dr Kawato said that neuroimaging biomarkers may soon become a clinical reality and he hoped that machine learning algorithms based on biomarkers might also find a place as another modality in the management of psychiatric disorders.